Telemedicine and Offshoring: Expanding Access to Healthcare Globally
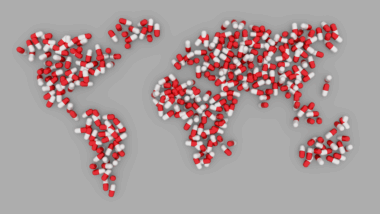
Telemedicine has revolutionized the way healthcare is delivered, enabling practitioners to provide services remotely via technology. This innovation is not just about convenience; it’s about breaking down geographical barriers. Offshoring in healthcare involves transferring certain medical functions or services to foreign countries, capitalizing on cost-effective solutions without compromising quality. As practitioners embrace telemedicine, offshoring becomes a more viable option. By leveraging telemedicine and offshoring, healthcare organizations can expand access to a broader population, especially in lesser-served regions. Patients can connect with specialists via video calls, reducing travel time and costs. This adaptability fosters better health outcomes, particularly for chronic disease management. For many, this service acts as a lifeline, giving access to precious medical advice and treatment from faraway locations, which may have been impossible otherwise. Furthermore, offshoring helps reduce operational costs significantly, freeing up resources for other critical areas in healthcare. Ultimately, the synergy between telemedicine and offshoring is expected to shape the future of global health by improving efficiency, reducing costs, and facilitating greater access to quality care for patients everywhere.
Offshoring plays a vital role in telemedicine’s adaptability, allowing healthcare providers to interact with patients worldwide from different locations. While the logistical challenges of offshoring persist, technological solutions have offered answers to issues like connectivity and security. Providers can use encrypted connections to ensure patient confidentiality while delivering high-quality services. Moreover, healthcare staff in offshore regions can receive specialized training, making them competent to assist in telemedicine. This dual advantage not only benefits patients seeking care but also enhances the skills of the workforce across the globe. Countries with a robust IT infrastructure are ideal candidates for offshoring healthcare services; thus, providers can tap into specialized skills while managing costs effectively. For instance, Indian healthcare professionals are often sought for their expertise in telemedicine, being fluent in English and equipped with technology. However, quality assurance remains paramount; organizations must establish guidelines and protocols governing offshored services diligently. This ensures that patients receive safe and effective care, fostering confidence in both telemedicine and offshoring, ultimately paving the way for a more connected healthcare ecosystem.
The Benefits of Telemedicine in Offshoring
Telemedicine juxtaposed with offshoring allows for numerous benefits that can greatly enhance patient care. First and foremost, it facilitates timely access to healthcare resources, particularly in emergency cases where immediate attention is required. Patients in remote areas can avoid long waits for appointments, eliminating geographical constraints. The operational costs associated with offshoring help practitioners maintain affordability for patients while ensuring staff are well-equipped to deliver quality services. Additionally, telemedicine ensures countless administrative burdens are managed effectively, leading to reduced overhead expenses. Practitioners can focus on patient care rather than back-office processes. The emphasis on preventive care becomes possible through routine check-ups, promoting healthier lifestyles and reducing subsequent healthcare costs. Also, patients can receive follow-up care efficiently and manage chronic conditions remotely, allowing for continuous management without the need for travel. Furthermore, telemedicine promotes cross-jurisdictional collaboration by enabling specialists from different regions to consult on cases collaboratively. Through this seamless integration of global expertise, offshoring positions healthcare systems to embrace modern challenges, setting the stage for a more integrated approach to future medical needs.
However, challenges accompanying offshoring in telemedicine cannot be overlooked. One significant hurdle lies in regulatory compliance, with various countries enforcing their own unique legislation regarding telehealth services. Navigating these laws becomes an arduous task, necessitating in-depth knowledge and skilled professionals to manage legalities. Ensuring consistent quality and care standards across different regions poses another challenge, as variations in education and training can lead to discrepancies in service delivery. Moreover, technology disparities can affect service availability, especially for patients in underdeveloped areas. Internet access is not universally equitable, and some patients may struggle with connecting to telemedicine services, limiting accessibility. Furthermore, cultural competency plays an essential role in telemedicine; healthcare providers must be sensitive to regional cultural nuances to build trust and rapport with patients effectively. Miscommunication can undermine the effectiveness of care, indicating that training must extend beyond clinical aspects. To succeed in achieving optimal outcomes, healthcare organizations must acknowledge and address these challenges while reaping the countless benefits that offshoring and telemedicine can offer, ultimately fulfilling their mission to serve patients better across the globe.
The Future of Telemedicine and Offshoring
The future of telemedicine, intertwined with offshoring, suggests a promising avenue for the evolution of global healthcare. As advancements in technology continue to emerge, the synergy between patient care and digital innovation will only deepen. With artificial intelligence poised to revolutionize diagnostics, offshoring healthcare could supply necessary support to clinicians, enabling them to deliver personalized treatment even more efficiently. The rise of wearables and health-tracking apps will augment telemedicine interactions, allowing for data-driven decisions and real-time health monitoring, which will enhance patient engagement. Furthermore, as telemedicine becomes more mainstream, regulatory frameworks will inevitably adapt. Governments might evolve policies to ensure that offshored services meet national healthcare standards, promoting patient safety and trust. Accordingly, establishing partnerships and networks across nations will be essential. Collaborative initiatives can strengthen the integration of offshored telemedicine, fostering knowledge sharing and skills development across diverse healthcare environments. Ultimately, the functional relationship between telemedicine and offshoring offers a unique opportunity to redefine healthcare delivery, bridging gaps and creating resilient systems that adapt to future healthcare demands globally.
Ultimately, the interplay of telemedicine and offshoring presents an innovative route to mitigating many challenges faced by modern healthcare systems. As patient populations continue to grow and diversify, healthcare delivery must become more adaptable and efficient. Offshoring enables healthcare organizations to scale their services without losing quality, harnessing global talent across multiple time zones. This leads to enhanced patient experiences as they gain access to specialists without geographical constraints. Furthermore, rising costs associated with traditional healthcare models have spurred a shift towards alternative solutions, making telemedicine and offshoring more appealing to buyers. Transitioning to a hybrid model allows organizations to maintain physical presence while implementing remote services effectively. Thus, stakeholders must be educated on the nuances of telemedicine and offshoring, maximizing resource allocation and ultimately improving patient care. As systems continue evolving and new technologies emerge, maintaining open lines of communication will be crucial for sharing insights and experiences. Therefore, regular assessments and adaptations will lead to the efficient integration of telemedicine and offshoring, creating optimized healthcare systems that cater to the needs of diverse populations.
Conclusion
In conclusion, the intersections of telemedicine and offshoring embody a powerful movement towards expanding healthcare access globally. They present opportunities for enhanced patient care from professionals who otherwise could not offer their services. Moreover, these platforms’ adaptability allows for personalized approaches, addressing specific health conditions efficiently. Stakeholders, including healthcare providers, patients, and policymakers, must embrace these innovations and adapt to the changing landscape. This involves continuous learning and adapting to technological advancements while ensuring strict adherence to the ethical implications involved in health services. Therefore, fostering collaboration and open communication between regions and stakeholders is essential. Telemedicine’s expansion into offshore spheres will nurture mutual respect for cultural differences, leading to effective patient outcomes. It’s imperative to recognize that while offshoring carries inherent challenges, the potential to improve healthcare access audaciously is undeniable. By committing to these evolving practices, organizations will not only enhance their operational efficiencies but will also help uplift under-served communities through better access to healthcare services. As the global healthcare landscape transforms, telemedicine and offshoring will likely remain central to discussions on the future of healthcare, driving innovation and equitable access.
The interplay between telemedicine and offshoring embodies a transformative shift in the healthcare landscape, presenting myriad possibilities for improving patient care across diverse populations. As healthcare systems increasingly embrace technological advancements, telemedicine offers a practical solution to help patients access medical expertise remotely. This model is especially beneficial in regions where healthcare resources are insufficient, enabling individuals to consult with specialists without the burden of travel. The offshoring aspect becomes pivotal in ensuring that higher quality and often more cost-effective services reach those in need. By utilizing international healthcare providers who are skilled in telemedicine, organizations can increase capacity and decrease waiting time for patients seeking effective treatment options. Thus, integrating telemedicine with offshoring strategies not only improves operational efficiencies but also enhances patient experiences, leading to better health outcomes overall. Furthermore, healthcare systems can effectively manage populations with chronic conditions through ongoing virtual consultations, reducing unnecessary hospital visits. This proactive approach to healthcare promotes healthier communities and instills confidence in patients seeking timely medical attention. Consequently, healthcare organizations that adopt these revolutionary practices will find themselves at the forefront of delivering accessible, high-quality services to varying demographics worldwide.